What is osteoarthritis
Osteoarthritis (ОА) is the most common form of arthritis and one of the fastest growing causes of disability in the world. Symptoms of osteoarthritis are systematically observed in 18% of women and 9.6% of men over the age of 60 years. About a quarter of these people are not able to carry out daily activities. Scientists predict that by 2050 up to 130 million people will suffer osteoarthritis which will significantly increase the social burden on the states.
The pathology of OA is multifactorial. It includes remodeling of the subchondral bone, inflammation of the synovial membrane of the joint, and damage to the articular cartilage.
Researchers in different countries have suggested that obesity, diabetes, and metabolic syndrome may directly contribute to the development of osteoarthritis. In turn, the treatment of OA today is largely limited only to the fight against its symptoms or the complete replacement of the joints. The international community officially recommends physical exercise and weight control as a therapy. But clinical practice shows that such treatment is often negligible.
Help yourself by yourself
In fact, patients with a diagnosis of OA can significantly affect the state of the disease through diet. British doctors from the University of Surrey reviewed current publications on the influence of food factors on the development of steoarthritis and summarized the findings. There are three main recommendations.
Move and lose overweight
Obesity increases strain on weight-bearing joints and, longitudinally, overweight and obese individuals are at considerably higher risk for knee arthroplasty. But extensive research by scientists from the Netherlands proves that there is also a non-mechanical connection between OA and obesity.
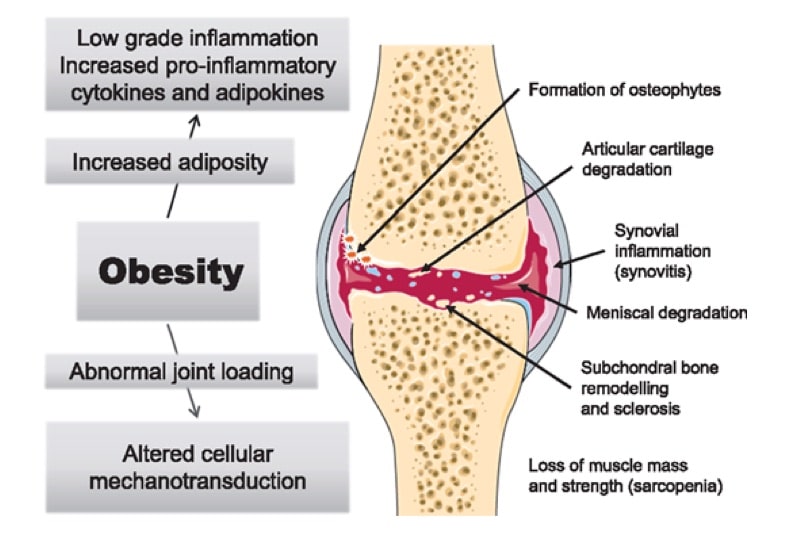
Fig.1 Mechanisms by which obesity leads to or exacerbates OA
Elevated Adipokines could comprise a critical link between obesity and OA. Leptin, an adipokine generally elevated in obesity and produced by white adipose tissue of the infra-patellar fat pad, may underlie this relationship. Leptin is associated with inflammation and degradation and may be involved in the pathophysiology of OA at the local and systemic level.
Reducing adipose tissue while maintaining muscle mass is very useful in osteoarthritis. Weight loss programs, as well as exercise, are much more effective against the disease than only physical exercise.
Eat a fat fish
Nutrition has an effect on systemic lipid levels (fatty acids). Therefore, it is likely that manipulation of the diet can significantly affect the cartilage tissue and disorders in osteoarthritis of the knee joints. An extensive study of patients with osteoarthritis has shown that a higher intake of saturated fat leads to a decrease in the volume of the joint cavity. At the same time, higher consumption of monounsaturated (MUFA) and polyunsaturated (PUFA) fatty acids (Omega-3 and Omega-6 acids belong to this group) was accompanied by a decrease in the radiographic progression of the disease.
One of the main components of lipids that mediate and regulate inflammation are eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA). They belong to Omega-3 acids. EPA / DNA create proinflammatory eicosanoids and mediators that reduce inflammation in osteoarthritis. Eicosanoids formed from Omega-6 acids in turn do not have such an anti-inflammatory effect.
Eicosanoids are oxidized derivatives of polyunsaturated fatty acids. Dietary sources of polyunsaturated fatty acids are seed oils and fish fat.
Modern diets are characterized by a high prevalence of Omega-6 over Omega-3 which stimulates inflammation. In the framework of the Melbourne collective study of healthy people, an association was found between increased consumption of Omega-6-containing products and the development of bone-marrow lesions. The highest content of Omega-6 acids in safflower (79%) and sunflower (62.2%) oils. The lowest content of Omega-6 acids among traditional seed oils is in olive oil which is rich in monounsaturated acids.
Mainly, EPA / DHA predominate in fish fat. The recommended intake of fat fish “at least one good serving per week” in a significant proportion of adults in developed countries is not observed. Consumption of EPA / DHA on the threshold of anti-inflammatory action in osteoarthritis can also be achieved by adding encapsulated fish fat to the diet. At the same time, scientists believe that there was no additional benefit of high-dose over low-dose fish fat in knee OA.
Thus, the researchers conclude that a diet that includes regular consumption of fish fat helps to reduce pain in osteoarthritis. The recommended dose of fat intake is equivalent to 1.5 capsules of 1 g of fish fat per day. These are about 3-4 servings of available sea fish of 150 g per week. Acceptance of encapsulated fish fat as an alternative must be treated carefully and purchase preparations only from reliable manufacturers.
Vitamin K and green leafy vegetables
Vitamin K is a group of fat-soluble compounds with two natural forms: vitamin K1 (phylloquinone) and vitamin K2 (menaquinone). Vitamin K1 is synthesized by plants and algae and is the form that is most widely present in the human diet. We meet it on the table mainly like green leafy vegetables and vegetable oils.
Vitamin K is involved in the mineralization of bones and cartilage. The lack of its consumption leads to a decrease in the carboxylation of vitamin K-dependent proteins entering the bone tissue. This in turn leads to anomalies that are very close to the symptoms observed in osteoarthritis.
Studies on the effects of vitamin K are very limited. For the most part they are devoted only to phylloquinone. But these studies demonstrate a positive relationship between the low concentration of phylloquinone and the development of osteoarthritis.
The unique relationship between vitamin K intake and the degree of development of osteoarthrosis has not yet been established. But the essential role of vitamin K in bone and cartilage health is undeniable. Not all groups of the population consume vitamin K at the recommended level but only about half of older people.
Conclusion
Despite the limited evidence based primarily on observations and related to OA of the knee, this review provides very specific recommendations for doctors and patients.
The global aging of the population and the modern scourge of obesity predict a vast increase in the incidence of osteoarthritis. Given the current lack of options for its treatment you should resort to any risk-free means to reduce the debilitating symptoms of the disease. Among the many recommendations of a healthy lifestyle and nutrition we can definitely identify those that have a beneficial effect on patients with OA. This is the fight against overweight with a diet in combination with the movement, as well as the consumption of fish fat and green vegetables in the recommended amount.
The overview of report “What is the evidence for a role for diet and nutrition in osteoarthritis?” by Sally Thomas, Heather Browne, Ali Mobasheri and Margaret P Rayman on ©Rheumatology. First published on 17 April 2018.

